By Douglas A. Drossman
From Stigma to Acceptance
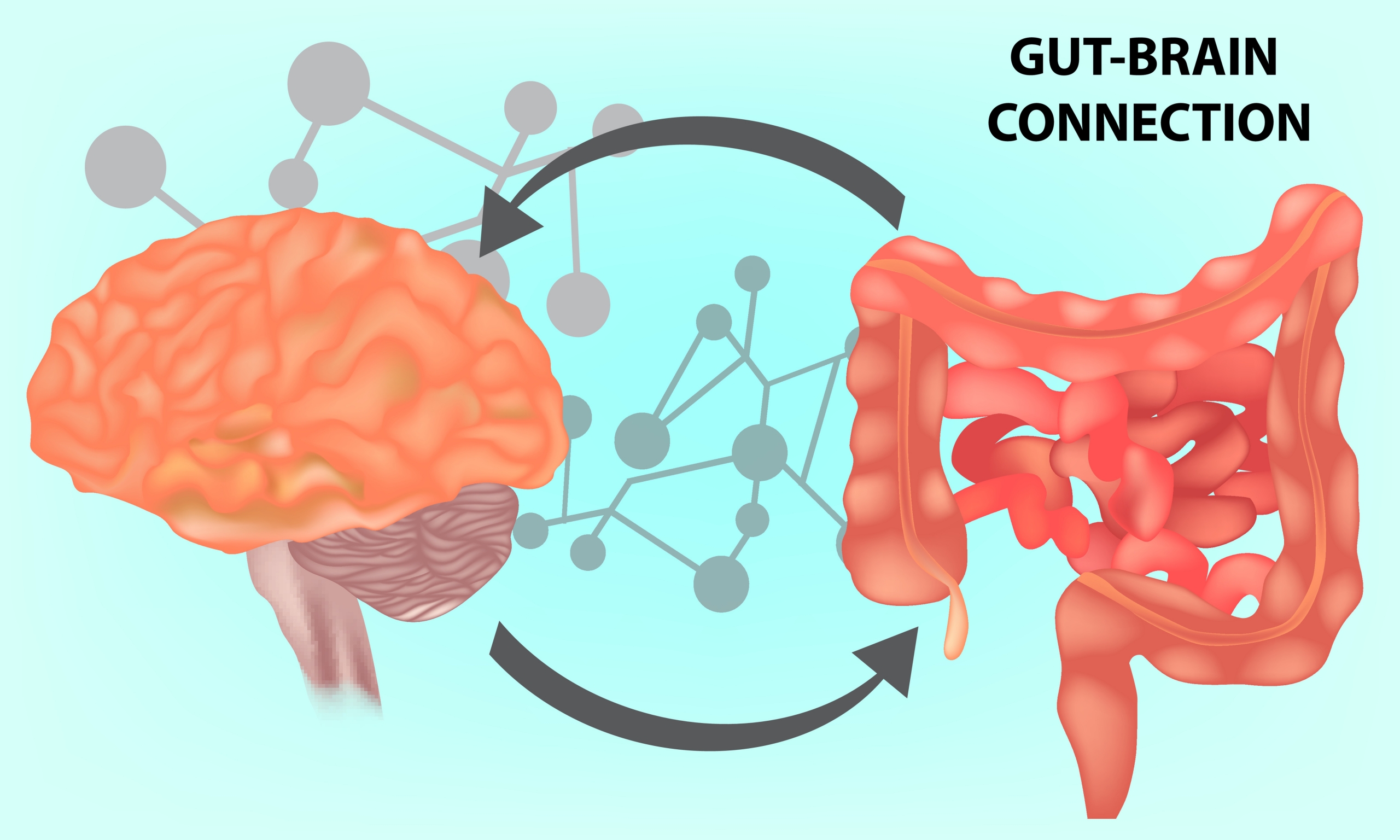
Recently, I was honored to do two interviews, one for the cover story of ACG magazine and the other, a podcast for the Healio series Gut Talk, by my fellow Rome board member William Chey. These honors allowed me the opportunity to stop and reflect on how the field, and with it, the Rome Foundation, has grown throughout my years as a clinician, educator and researcher. In the late 80s, I surveyed the AGA membership and found that most defined a Functional GI Disorder as ‘nothing found’ or ‘psychiatric disorder’. Since its founding in the early 1990’s, Rome Foundation has focused on changing this paradigm, eventually defining it as a disorder of gut-brain interaction. That has evolved from new research; Rome has always been on the cutting edge of this research in DGBI. I am proud to have contributed through Rome and through my research to overcome obstacles to recognizing DGBI as legitimate conditions, not imagined or psychiatric.
Finding the Patients
The first hurdle to getting recognition of DGBI was that the so-called ‘functional disorders’ were neither well understood nor categorized. People didn’t understand them and didn’t care. Moreover, clinicians struggled to handle these patients with no structural abnormalities suffering from severe symptoms while being confused about why patients with Crohn’s disease having the same symptoms were considered legitimate in their complaints. Only after these patients were identified and categorized could the study of these so-called ‘functional disorders’ begin. The identification began in the 1990’s through the use of symptom-based criteria championed by the Rome Foundation. Of course, once studied and categorized as clinical entities, they became legitimate.
Finding the Evidence
Although aspects of brain-gut interactions in DGBI are now better recognized and understood, the prevalent idea in my early career was that there must be an organic cause for the symptoms. Research focused on finding that structural defect. The paradigm shift began with the Manning Criteria publication in 1977, a precursor of the Rome Criteria. Then under the direction of the late Aldo Torsoli, a panel of international experts was encouraged to form a working team, which was the Rome Foundation’s genesis in retrospect. We published the first working team report “Irritable Bowel Syndrome: Guidelines for the Diagnosis” in 1989. Our goal was to fight back against the narrative that nothing is wrong if it’s not seen in a test. This helps neither doctors nor their patients struggling to function in their daily lives. Symptom-based criteria allowed us to understand the patients’ symptoms, regardless of the presence of structural or physiological findings.
By the late 80s, we had begun conducting clinical and epidemiological research to characterize the symptoms and better understand the mechanisms at work in DGBI. A year after the first working team report, a second report, “Identification of Subgroups of Functional Intestinal Disorders”, was published, which categorized the DGBI (then called Functional Intestinal Disorders) and allowed for better diagnoses and more targeted treatments.
The next big breakthrough came from an interesting phenomenon I noticed in my clinic: the prevalence of a history of trauma in GI patients. This led to an NIH grant producing research publications that spanned 25 years. For the first time, a medical team studied the link between trauma and symptom severity. This led to more and more biopsychosocial research as well as the study of visceral hypersensitivity, food and diet, the microbiome and more. As a result of the breakthroughs of many others over the last 2 decades, we now understand Disorders of Brain-Gut to be based on 1) motility disturbance, 2) visceral hypersensitivity, 3) altered mucosal and immune function, 4) altered microbiota, and 5) altered CNS processing. Because of this research’s legitimacy, the use of symptom-based criteria has since spread because clinicians have recognized it as more cost-effective, scientifically accurate and less stigmatizing to the patients.
Spreading the Word
Once the research pointed to new pathophysiology and provided new treatment options, the next obstacle was to get this information into clinical practice. Most medical students are never given communication skills training, with a particularly disastrous effect on the experience of patients with DGBI. It’s not what you say with these patients, but how you say it that makes a difference in the outcome. And most providers are given only minimal training in diagnosing and treating DGBI. To that end, Rome has expanded its activities over the past few years to include training and educational programs, grounded in the biopsychosocial model first described by my mentor, George Engel. Before COVID, we facilitated workshops all over the country led by experts in the field, and now these programs are available online through Rome’s online campus.
Looking Ahead
What started as clinical trials guidelines to create a patient population to study has since expanded to something much larger. Equally exciting to me is how many new clinicians and researchers are coming to the field through Rome’s activities. Only two years ago, Rome launched a GI Psych section headed by Laurie Keefer and Sarah Kinsinger, which now has nearly 400 members. My program DrossmanCare produces videos and educational programs to teach communication skills. We have now partnered with the Rome Foundation to develop a curriculum for learning Communication skills: “What Do You Hear” and have produced a book just released Gut Feelings: Disorders of Gut-Brain Interaction and the Patient-Doctor Relationship, A Guide for Patients and Doctors. The Rome Foundation Research Institute, under Magnus Simren, is working to advance scientific understanding of the disorders of gut-brain interaction. Currently, three studies are underway, with several more planned. Thousands of providers all over the world have access to training through the Rome Campus, our new educational initiative. And most importantly, Rome is updating its work. Rome V is currently in the early planning phases and will be published in 2026. Our goal will be to integrate new knowledge into an expanding database of knowledge. I anticipate we will identify biomarkers to provide more targeted treatments to help our patients with DGBIs, a “real” set of disorders.
 5826 Fayetteville Rd., Suite 201 Durham, NC 27713
5826 Fayetteville Rd., Suite 201 Durham, NC 27713  (919) 246-5611
(919) 246-5611