In the course of my practice and in my care for my patients, I believe that one of the most important items of information that comes up in my discussions with each patient relates to whether his or her problem will get better or are we just “treating the symptoms”.
In these discussions, I address the concept of neurogenesis or brain cell growth. I have learned that this is very new information for most patients and even for the physicians they have seen, even physicians who refer patients to me.
This first slide illustrates the theory of neurogenesis showing how illness and bad stuff suppresses neurogenesis in the hippocampus (on bottom), then treatment restores it.
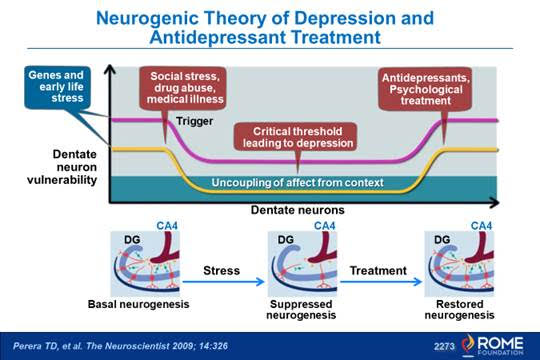
This is new research having existed for only about a decade and to many patients and physicians it even seems counterintuitive.
Why?
When I was in medical school I was taught that brain cells don’t grow after a young age. I mention this to you because the idea of neurogenesis relates to my practice of seeing patients with functional GI disorders and chronic pain.
I will often use or prescribe centrally targeted treatments (antidepressants, other neuromodulators, cognitive behavioral treatment, hypnosis, among others) to help reduce the symptoms of the chronic GI conditions including abdominal pain and its associated emotional distress.
Yes, these treatments can help mood and it does help pain in the right combination and dosage after only a few weeks, but when used for longer periods (6 months to 2 years) it also can lead to neurogenesis.
In discussions with my patients, I give examples of studies in laboratory animals where these treatments lead to regrowth of nerves and discuss brain imaging studies in humans that support this concept. These two slides show how brain damage to the rat reduced performance in a maze compared to control groups but then when treating with an antidepressant, those rats did better and weeks later their brain cells showed brain cell growth.
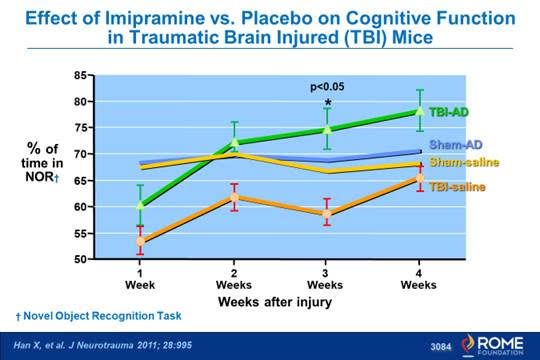
This graph shows reduced performance in a maze of mice that had brain injury (orange line ) compared to the controls (yellow and blue lines). However rats that received brain damage who also were put on an antidepressant (imipramine – green line)) did even better than controls.
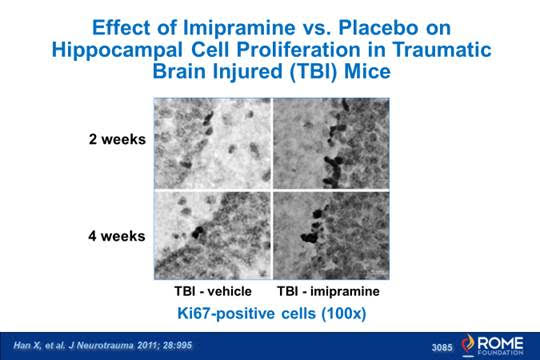
This slides shows brain cell precursor growth (dark staining of the cells) of mice that had brain damage at 2 weeks and four weeks. Note that the imipramine treated group on the right had darker staining indicating greater precursor brain cell activity (neurogenesis).
When new brain cell growth occurs, we can now talk about re-establishing dysfunctional neural connections between the brain and gut. This can allow us to reduce or even stop some of the medications and reverse a patient’s condition, such a pain or depression. We call that relapse prevention.
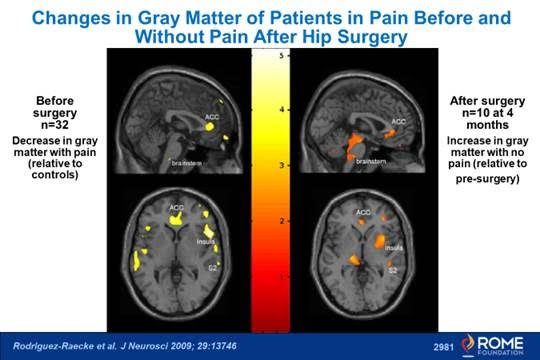
This last slide is very interesting – it shows that patients with chronic hip pain have reduced cell density (presumably nerve cell loss) in the pain control areas but after hip replacement and the pain goes away you see increased density (nerve cell growth) showing how chronic pain can suppress neurogenesis and how pain relief (as we can do with meds) leads to neurogenesis.
I just came across an interesting TED talk by Sandrine Thurot Ph.D, who is a stem cell researcher in England who I believe can provide further insight into this concept. Watch the Video
Three Tips You Should Know
-
There are lifestyle things you can do as in the video to help promote neurogenesis
-
There are lifestyle things you shouldn’t do as in the video that may suppress neurogenesis
-
If you don’t get a response in your pain after several weeks of treatment, stay with it, as the neurogenesis effect can take months to a year or two.
In addition I am glad to provide additional reading material on this topic or discuss it further with you.
Watch the Video
I hope you will enjoy and learn from it.
Douglas A. Drossman MD
 5826 Fayetteville Rd., Suite 201 Durham, NC 27713
5826 Fayetteville Rd., Suite 201 Durham, NC 27713  (919) 246-5611
(919) 246-5611 