A motility disorder is an abnormality in the coordination of the muscles of the gastrointestinal tract. Motility disorders are defined by abnormalities of pressure waves generated during gastrointestinal functioning. When the normal functioning is impaired there may be increased or decreased motility and this can also produce pain. Examples would be gastroparesis (impaired and slowed emptying of the stomach), pseudo-obstruction (slowing of the intestines), or abnormal emptying of the rectum (dyssynergic defecation). Motility disorders are defined by impairment of the muscular system of the gastrointestinal tract and there may or may not be symptoms.
“Motility” is an unfamiliar word to many people; it is used primarily to describe the contraction of the muscles in the gastrointestinal tract. Because the gastrointestinal tract is a circular tube, when these muscles contract, they close off the tube or make the opening inside smaller – they squeeze. These muscles can contract in a synchronized way to move the food in one direction (usually downstream, but occasionally upstream for short distances); this is called peristalsis. If you looked at the intestine, you would see a ring of contraction that moves along pushing contents ahead of it. At other times, the muscles in adjacent parts of the gastrointestinal tract squeeze more or less independently of each other: this has the effect of mixing the contents but not moving them up or down.
The gastrointestinal tract is divided into four distinct parts: the esophagus, stomach, small intestine, and large intestine (colon). They are separated from each other by special muscles called sphincters which normally stay tightly closed and which regulate the movement of food and food residues from one part to another. Each part of the gastrointestinal tract has a unique function to perform in digestion, and as a result each part has a distinct type of motility and sensation. When motility or sensations are not appropriate for performing this function, they cause symptoms such as bloating, vomiting, constipation, or diarrhea which are associated with subjective sensations such as pain, bloating, fullness, and urgency to have a bowel movement. You can learn about the normal patterns of motility and sensation in each part of the gastrointestinal tract using the following links. Also there is information about the symptoms that can result from abnormal motility or sensations.
Normal Motility and Function
The function of the esophagus is simply to transport food from the mouth to the stomach, and powerful, synchronized (peristaltic) contractions follow each swallow to accomplish this task. Between swallows, the esophagus usually does not contract. There is a sphincter muscle separating the esophagus from the stomach (called the lower esophageal sphincter) which normally stays tightly closed to prevent acid in the stomach from washing up into the esophagus. However, when we swallow, this sphincter muscle opens up (relaxes) so that the food we swallow can enter the stomach.
Gastroesophageal Reflux Disease
The most common symptom that occurs in the esophagus is heartburn, which is caused when acid washes up into the esophagus repeatedly (gastroesophageal reflux) and irritates the lining of the esophagus. This happens when the sphincter separating the stomach from the esophagus does not work properly; the function of this sphincter is to prevent reflux from occurring when the stomach contracts. This can be due to a weak sphincter muscle, to too-frequent spontaneous relaxation of the sphincter, or to
hiatal hernia. Hiatal hernia means that the stomach pulls up into the chest above the sheet of muscle that separates the abdomen from the chest (this muscle sheet is called the diaphragm). A hiatal hernia weakens the sphincter. Gastroesophageal reflux disease may be diagnosed by an ambulatory pH study, which is a recording of the frequency with which acid washes up into the esophagus. It is done by putting a small, soft tube with one or two acid sensors on it down through your nose into your esophagus and connecting it to a battery-operated computer for 18-24 hours. You can go about your usual work and social activities during this test.
Dysphagia
Dysphagia means ineffective swallowing. Sometimes this occurs because the muscles of the tongue and neck that push the food into the esophagus are not working properly because of a stroke or a disease affecting the nerves or muscles of the tongue and throat.
However, food can also stick because the lower esophageal sphincter does not relax to let the food into the stomach (a disorder called achalasia) or because the esophagus contracts in an uncoordinated way (a disorder called esophageal spasm). Dysphagia can cause food to back up in the esophagus and lead to vomiting. There may also be a sensation of something getting stuck or a sensation of pain. Tests for dysphagia include esophageal manometry, which means that a small tube containing pressure sensors is put down through the nose into the esophagus to measure the contractions of the esophagus and the relaxation of the lower esophageal sphincter. This test lasts about 30 minutes.
Stomach
Normal Motility and Function
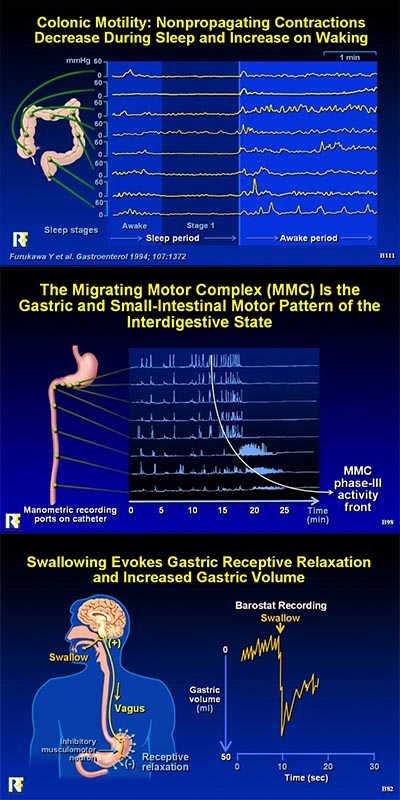
One function of the stomach is to grind food down to smaller particles and mix it with digestive juices so that it can be absorbed when it reaches the small intestine. The stomach also empties its contents into the intestine at a controlled rate. The stomach has three types of contractions: (1) There are rhythmic, 3 per minute, synchronized contractions in the lower part of the stomach which create waves of food particles and juice which splash against a closed sphincter muscle (the pyloric sphincter) to grind the food down into small particles. (2) The upper part of the stomach shows slow relaxations lasting a minute or more that follow each swallow and that allow the food to enter the stomach; at other times the upper part of the stomach shows slow contractions which help to empty the stomach. (3) Between meals, after all the digestible food has left the stomach, there are occasional bursts of very strong, synchronized contractions that are accompanied by opening of the pyloric sphincter muscle. These are sometimes called “housekeeper waves” because their function is to sweep any indigestible particles out of the stomach. Another name for them is the migrating motor complex.
Delayed Gastric Emptying (Gastroparesis)
The symptoms of delayed gastric emptying include nausea and vomiting. Poor emptying of the stomach can occur for several reasons: (1) The outlet to the stomach (the pylorus and duodenum) may be obstructed by an ulcer or tumor or by something large and indigestible that was swallowed. (2) The pyloric sphincter at the exit to the stomach may not open enough or at the right times to allow food to pass through. This sphincter is controlled by neurological reflexes to ensure that only very tiny particles leave the stomach and also to insure that not too much acid or sugar leaves the stomach at one time, which could irritate or injure the small intestine. These reflexes depend on nerves which sometime become damaged. (3) The normally rhythmic, 3/minute contractions of the lower part of the stomach can become disorganized so that the contents of the stomach are not pushed towards the pyloric sphincter. This also usually has a neurological basis; the most common cause is long-standing diabetes mellitus, but in many patients the cause of delayed gastric emptying is unknown, so the diagnosis given is idiopathic (meaning cause unknown) gastroparesis.
Tests used to evaluate patients with delayed gastric emptying usually include endoscopy to look inside the stomach, and gastric emptying (a nuclear medicine study) to measure how quickly food leaves the stomach. The test of gastric emptying involves eating food that has a radioactive substance added to it, so that the rate of emptying of the stomach can be measured with a type of geiger counter (gamma camera). Another, less frequently used tests is the electrogastrogram which measures small electrical currents that come from the stomach muscle and that indicate whether the 3/min contractions of the lower stomach are occurring normally. The contractions of the stomach can also be measured directly by passing a tube with pressure sensors on it down the nose and into the stomach.
Normal Motility And Function
The parts of the small intestine are the duodenum, jejunum, and ileum, but these three areas of the small intestine all have the same general function, namely the absorption of the food we eat. During and after a meal, the intestine normally shows very irregular or unsynchronized contractions which move the food content back and forth and mix it with the digestive enzymes that are secreted into the intestine. These contractions are not entirely unsynchronized; they move the contents of the intestine slowly towards the large intestine. It normally takes about 90-120 minutes for the first part of a meal we have eaten to reach the large intestine, and the last portion of the meal may not reach the large intestine for five hours. This pattern of motility is called the “fed (or eating) pattern.” Between meals, the intestine shows cycles of activity that repeat about every 90-120 minutes. These are easiest to see at night when there is a longer
period between meals, because meals suppress these cycles. The cycle consists of a short period of no contractions (Phase I), followed by a long period of unsynchronized contractions that appear similar to the fed pattern (Phase II), and then a burst of strong, regular contractions that move down the intestine in a peristaltic fashion (Phase III). Phase III represents a continuation of the “housekeeper waves that start in the stomach, and its function is to sweep undigested food particles and bacteria out of the intestine and into the large intestine.
There are two other kinds of motility seen in the small intestine, but their function is not as well understood. Discrete clustered contractions are brief bursts of contractions (each burst lasts only a few seconds) which are synchronized (peristaltic). They occur mostly in the upper small intestine and fade out before moving too far downstream. They occur in most people at infrequent intervals, but in patients with irritable bowel syndrome they may be associated with abdominal pain.
The second type of contraction is the giant migrating contraction. This occurs primarily in the lower small intestine (ileum), and it is peristaltic over long distances. It may be part of a defensive reflex that sweeps bacteria and food debris out of the intestine. These giant migrating contractions occur in healthy people and usually cause no sensation, but in patients with IBS they are frequently associated with reports of abdominal pain.
Intestinal Dysmotility, Intestinal Pseudo-Obstruction
Abnormal motility patterns in the small intestine can lead to symptoms of intestinal obstruction (blockage). These symptoms are bloating, pain, nausea, and vomiting. They vary in how severe or how frequent they are, but there are usually periods during which the patient is free of symptoms. These symptoms can result either from weak contractions or from disorganized (unsynchronized) contractions.
Weak contractions of the small intestine are due to abnormalities in the muscle and are usually associated with diseases such as scleroderma. These connective tissue disorders may cause the intestine to balloon out in places so that the contractions of the muscle are not able to move the contents downstream. Other patients have contractions that are strong enough, but they are too disorganized or nonperistaltic to move food along. This type of motility disorder is due to abnormalities in the nerves which coordinate (synchronize) the contractions of the intestine. This abnormality is easiest to detect by recording the housekeeper waves because these are easily identified peristaltic contractions. In intestinal pseudo-obstruction of the neurological variety, these bursts of contractions occur simultaneously over large parts of the intestine or they may actually move upstream. Another cause of dysmotility is intestinal pseudo-obstruction, which is not obstruction but poor motility. The test which is used to detect either of these intestinal motility abnormalities is a small bowel motility study. This involves putting down a long tube with pressure sensors on it which passes through the stomach and into the small intestine.
It is important to record several of the housekeeper wave fronts to be sure of the diagnosis. In some clinics this is done by recording for five hours or more while the patient lies on a bed in the clinic, but in other clinics, the pressure sensors are connected to a battery-operated computer and the patient is sent home to return the next day.
Small Bowel Bacterial Overgrowth
This means that there are too many bacteria in the upper part of the small intestine. This leads to symptoms of bloating, pain, and diarrhea that occur immediately after eating because the bacteria in the intestine begin to consume the food in the small intestine before it can be absorbed. These bacteria give off hydrogen and other gases which cause bloating and diarrhea. Small bowel bacterial overgrowth is a result of abnormal motility in the small intestine; when the housekeeper waves do not keep the bacteria swept out because the contractions are too weak or disorganized, the bacteria grow out of control.
Bacterial overgrowth is most easily detected by the hydrogen breath test: The patient drinks a sugar solution and breathes into a bag every 15 minutes for two hours. If the bacteria are present in large amounts in the small intestine, they give off hydrogen, some of which is absorbed into the blood, carried to the lungs, and breathed out where it can be detected.
Normal Motility And Function
The primary functions of the large intestine are to store food residues and to absorb water. Between what we drink and what is secreted into the stomach and intestine to help with food absorption, about 5 gallons of fluid is dumped into the large intestine every day. Most of this fluid has to be reabsorbed to prevent us from becoming quickly dehydrated. This process takes time, and as a result, about 95% of the contractions of the colon are unsynchronized (nonperistaltic). These contractions mix the contents of the large intestine back and forth but do not move them forward. As a consequence of this pattern of motility, food residues remain in the colon on average about 30 hours, and there are a lot of bacteria. The amount of bacteria varies depending on diet and use of antibiotics but can make up more than half of the weight of fecal material.A second and very important type of motility that occurs in the large intestine is the high amplitude propagating contraction (HAPC). These contractions only occur 6-8 times per day in healthy people, but they are extremely strong contractions which begin in the first part of the large intestine and sweep around all the way to the rectum; they stop just above the rectum. These contractions move the contents of the large intestine ahead of them, and they will often trigger a bowel movement, or at least the urge to have a bowel movement. Very slow contractions such as those seen in the upper part of the stomach (changes in muscle tone) also occur in the large intestine and may be important in its function, but there have not been studied enough to know for certain what they do.
The symptoms of constipation are infrequent bowel movements, passage of hard stools, and sometimes difficulty in passing stools. The sensations associated with constipation can include a constant feeling of needing to go, which can be very annoying, or a sensation of bloating or fullness. In children, constipation often leads to fecal incontinence. One of the two motility problems that can lead to constipation is a decrease in the number of high amplitude propagating contractions in the large intestine. The test used to detect this is a transit time (also called a Sitzmark) study, which is done very simply: the patient swallows some small rings which can be detected on an xray. In our clinic, the patient swallows 24 rings per day for 5 days and a single xray is taken on the sixth day. The time it takes for fecal material to move through and out of the large intestine can be estimated by counting the number of rings remaining on the sixth day.
Diarrhea
The symptoms of diarrhea are frequent, loose or watery stools and a subjective sense of urgency. Patients with diarrhea also may worry about loss of control over bowel movements. An excessive number of high amplitude propagating contractions can be a cause of diarrhea; it reduces the amount of time food residues remain in the large intestine for water to be reabsorbed. Changes in the motility of the small intestine may also occur, but there is little information available on this. It is usually not necessary to perform tests to document the motility disorder associated with diarrhea, but your doctor may want to collect a stool sample to evaluate other causes for diarrhea. A symptom diary in which you record the
number of bowel movements and rate their consistency (watery, loose, formed, etc.) for 1-2 weeks can be very helpful to your doctor in deciding on the most appropriate treatment.
Rectum and Pelvic Floor
Normal Motility And Function
The primary functions of the rectum and pelvic floor muscles are to prevent incontinence (loss of control) and to allow defecation to occur. The rectum is very elastic, which allows it to store food residues prior to a bowel movement, but it must also be stiff enough to funnel food residues towards the anus during a bowel movement. The rectum is also surrounded by sensory nerves that detect the filling of the rectum with food residues. This sensation of rectal filling enables us to consciously or unconsciously squeeze the external anal sphincter to prevent incontinence until we can reach a toilet.
These sensory nerves are also involved in reflexes that let the sphincter muscles relax during a bowel movement.
Fecal Incontinence
Fecal incontinence means involuntary passage of fecal material in someone over the age of 4 years. The most common causes are (1) weakness of the anal sphincters muscles that allow us to voluntarily hold back a bowel movement; (2) loss of sensation for rectal fullness so we can’t tell when to squeeze the sphincter muscles; (3) constipation, in which the rectum fills up and overflows; and (4) stiff rectum, in which the fecal material is forced through the rectum so quickly that there is no time to prevent incontinence by squeezing the sphincter muscles. Diarrhea can also lead to fecal incontinence.
Weakness of the sphincter muscles can result either from injuries to the pelvic floor muscles themselves or injuries to the nerves to these muscles. Delivering a baby is one of the most common causes of injuries to the muscles or nerves of the pelvic floor, but birth defects such as spina bifida and diseases such as diabetes mellitus and myesthenia gravis can also affect these nerves. Ulcerative colitis or other diseases that are associated with an inflammation of the rectal lining can cause a stiff rectum. Constipation with overflow incontinence is very common as a cause of fecal incontinence in children.
The medical evaluation to determine the cause of fecal incontinence will usually include a rectal manometry study in which a tube with a balloon on its tip is put into the rectum.
The tube has sensors on its sides to measure pressures in the area of the sphincter muscles. This test provides information on rectal sensation, stiffness of the rectal wall, and strength of the sphincter muscles. An electromyographic (EMG) test may also be performed to determine whether there is any damage to the nerves which go to the anal sphincters. A special type of ultrasound study is also frequently done to find out whether there are tears in the sphincter muscles.
Hirschprung’s disease
There are actually two anal sphincter muscles: an internal anal sphincter which is a part of the intestines, and an external anal sphincter which is part of the pelvic floor muscles.
The internal anal sphincter normally stays closed to prevent the leakage of gas or liquid from the rectum, but when the rectum fills up with gas or fecal material, a reflex causes it to open to allow the bowel movement to pass through. The nerves that this reflex depends on are sometimes missing at birth, with
the result that the internal anal sphincter stays tightly closed and bowel movements cannot occur. This congenital (birth) defect is called Hirschprung’s disease. It can be detected by rectal pressure measurements showing that the internal sphincter does not relax when the rectum is distended by a balloon.
Alternatively, Hirschprung’s disease can be diagnosed by snipping off a part of the lining of the rectum to check for the presence of the nerve cells.
Outlet Obstruction Type Constipation (Pelvic Floor Dyssynergia)
The external anal sphincter, which is part of the pelvic floor, also normally stays tightly closed to prevent leakage. When you try to have a bowel movement, however, this sphincter has to open to allow the fecal material to come out. Some people have trouble relaxing the sphincter muscle when they are straining to have a bowel movements, or they may actually squeeze the sphincter more tightly shut when straining. This produces symptoms of constipation. The medical evaluation for this type of constipation will usually begin with the type of anal manometry and/or pelvic floor electromyographic tests that are described above. However, another useful test is put a small balloon or some thick pasty material into the rectum and test whether the patient can pass it. The first test is called the balloon defecation test, and the second test is called defecography.
Summary
The gastrointestinal tract is divided into four distinct parts which are separated by sphincter muscles; these four regions have distinctly different functions to perform and different patterns of motility (contractions). They are the esophagus (carries food to the stomach), stomach (mixes food with digestive enzymes and grinds it down into a moreor less liquid form), small intestine (absorbs nutrients), and colon (reabsorbs water and eliminates undigestible food residues). Abnormal motility or abnormal sensitivity in any part of the gastrointestinal tract can cause characteristic symptoms: food sticking, pain, or heartburn in the esophagus; nausea and vomiting in the stomach; pain and bloating in the small intestine; and pain, constipation, diarrhea, and incontinence in the colon and rectum. There are tests to determine whether the motility (contractions) in each part of the gastrointestinal tract are abnormal, and these tests provide guidance to the physician or surgeon in how best to treat these symptoms.
 5826 Fayetteville Rd., Suite 201 Durham, NC 27713
5826 Fayetteville Rd., Suite 201 Durham, NC 27713  (919) 246-5611
(919) 246-5611 